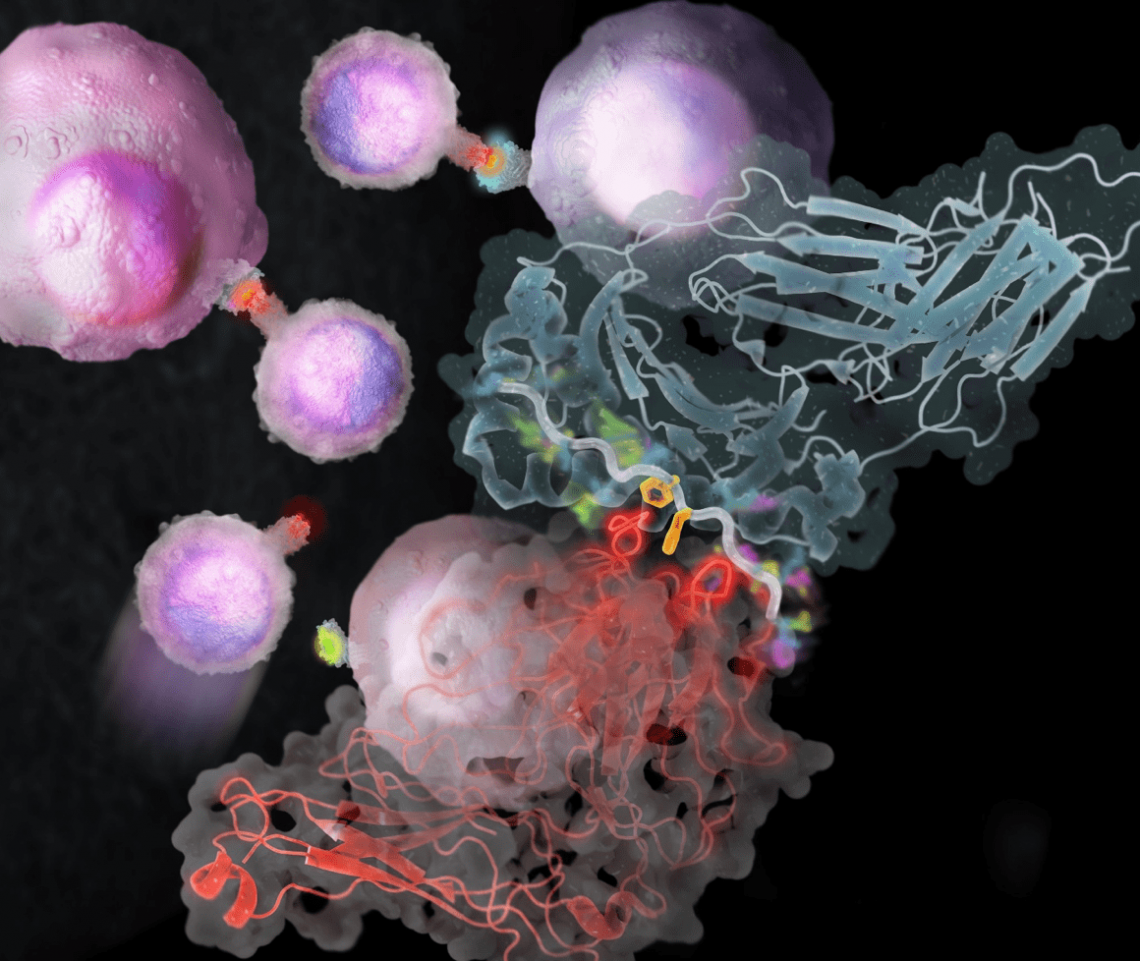
Immune checkpoint inhibition and chimeric antigen receptor T cell treatments have recently achieved clinical success, signaling a watershed moment in cancer immunotherapy. These outcomes also highlight the necessity of knowing fundamental tumor immunology for successful clinical translation in cancer treatment. The Reviews in this Review Series emphasize recent improvements in our understanding of basic features of tumor immunology and indicate how these insights might lead to the creation of novel immunotherapeutic techniques.
Understanding how cancer interacts with the immune system is critical for delineating the fundamental foundation for cancer immune evasion and designing successful immunotherapies. Over the last decade, data from mouse models and human cancer patients has accumulated demonstrating the relevance of the immune system in identifying and removing altered malignant cells. The immune system also plays an important role in tumor growth. Cancer immunoediting refers to the immune system’s dual involvement in suppressing and/or promoting cancer development, and it consists of three stages: elimination, equilibrium, and escape.
Dr. Paul E. Love, an NIH investigator from Bethesda, Maryland, is investigating whether human T Cell Antigen Receptor (TCR) signaling components and TCR signal-altering proteins might be used as immunotherapy targets. This study, which might lead to a significant advancement in immunotherapy, focuses on the TCR’s signaling apparatus, which is responsible for the activation of T cells, which are important for pathogen resistance and tumor monitoring. As a researcher, Dr. Love has more than 31 years of expertise. He specializes in immunology and has a long list of publications in fundamental science and medicine to his name. Dr. Love works at the National Institute of Health (NIH), which is part of the US Department of Health and Human Services.
He is still a key figure at the NIH, having served as a Senior Investigator for almost 25 years. Dr. Love is the director of an immunology laboratory at the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). He possesses both a Ph.D. and an MD, and he is board certified in Clinical Pathology. After finishing his residency at Washington University, he became a fellow in Human Genetics at the National Institute of Health.
Applied research makes use of results from basic research to promote public health, primarily through adapting basic discoveries to the treatment of human ailments. Applied research has identified checkpoint molecules such as Ctla4, PD-1, and PD-L1, which are employed to reduce or halt cell-T activation. Blocking checkpoint molecules was demonstrated to lead to improved tumor death by T cells in basic mouse tests. This discovery changed human cancer treatment and paved the way for immunotherapy, a new and fascinating field of medicine.
Two study lines in Dr. Love’s lab have identified potential translational uses of fundamental research in human medicine. One line focuses on the structure and function of the TCR, with a particular focus on the immune-receptor-tyrosine-based activation-motives (ITAMs) signal-transducing modules found within the TCR’s six signal transducing subunits. Dr. Love’s team is looking at whether changing the TCR ITAM sequences might increase cell activation and function, particularly tumor cell killing. As a result, the goal of this research is to see if TCR signal transducing subunits can be ‘tuned’ to improve TCR-mediated cell activation and tumor death. The second line of study is to define and characterize a family of chemicals known as tuning molecules, which function to attenuate TCR signals operating on cells.